
Appendicitis: Imaging andAlternative Diagnoses
Mindy M. Horrow, MD, FACR, FSRU
January, 2013
Director of Body Imaging
Einstein Medical Center
Professor of Radiology
Thomas Jefferson University Medical School

Background
Most common cause ofabdominal pain requiring surgery
Rare in the past and inunderdeveloped countries
Prompt diagnosis minimizesmorbidity and mortalityassociated with perforation

Anatomy
Diverticulum approx 10 cm arisingfrom post-med cecum, approx 3 cmbelow ileocecal valve. Variablelocation influences presentation.
Location of base constant, butremainder is free: retro or sub cecal,retro or pre ileal, pelvic. May ascendto right lobe of liver

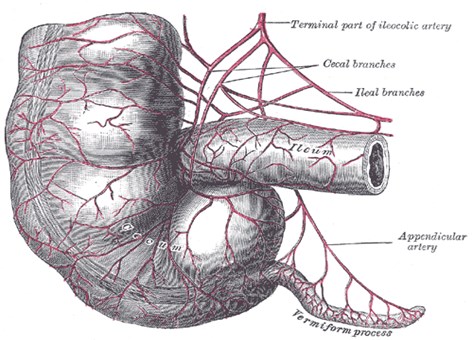
From Gray’s Anatomy

Pathophysiology
Luminal obstruction secondary tofecalith, lymphoid hyperplasia, foreignbody, parasite, primary and secondarytumors
Fecaliths in 11-52%, true calculi lesscommon but associated more withperforation
After obstruction, mucus secretioncontinues with luminal distention

Pathophysiology
Distention stimulates visceral nervesresulting in ill-defined epigastric pain,nausea, vomiting (4-6 hours)
Vascular engorgement leads toischemia and transmural inflammationwhich extends to peritoneum. Thissomatic pain localizes to appendix.
Afebrile or low grade fever
Higher fevers, consider perforation(may be walled off or into peritoneum)

Types of Appendicitis
Mild appendicitis may resolve if obstruction isrelieved
Recurrent appendicitis: multiple, similarattacks of RLQ pain leading to appendectomy,CT and surgical findings of acute appendicitis,occuring in 7% cases of acute appendicitis
Chronic appendicitis: RLQ pain at least 3weeks, no other diagnosis, histologic findingsof chronic, active inflammation or fibrosis,surgery cures symptoms
Unrecognized malignancy in 0.5 – 1% surgicalspecimens for appendicitis

Clinical Diagnosis
Classic presentation in 60%
Diagnosis may be missed or delayed ifatypical location of appendix, extremesof age, pregnancy
Overall clinical accuracy = 80%resulting in false negative surgery in20%, reached clinical plateau in mid-1980s
Accuracy in men: 78-92%
Accuracy in women: 58-85%

Perforation
Overall incidence of 20%
Highest in very young and old (40-70%)
Conventional surgical wisdom basedupon inverse relationship betweenfalse-negative appendectomy rate andperforation rate. This justifies FNappendectomy rate of 15-23%.However, may not be true.
Perforation correlates with time ofonset of symptoms to treatment

Visualization of Normal Appendix
Mean frequency of visualization of normal appendix atun-enhanced CT : 79%
Mean frequency of visualization after rectal contrast :90-100%
Mean thickness when contents are not visualized(cannot be subtracted) : 6.6mm (range, 4.0-11.0mm)
Mean thickness when contents are visualized (can besubtracted) : 3.6 mm (range, 2.0-6.0)
Location of appendiceal tip: 62% paracolic, 19% pelvic,9% midline, 10% retrocecal, <1% subhepatic
Benjaminov, etal. Radiology 2002; 225:400

Visualization of Normal Appendix
Reproducibility of identification of appendix
–increases with BMI and increasing abdominal fat
–Depends upon position
–Depends upon gas within lumen
–Does not depend upon enhancement
Visualization and confidence increases withthinner reconstruction sections.
Keyzer, etal. AJR 2008;191:507
Johnson, etal. AJR 2009;192:833

Visualization of Normal Appendix
Frequency of visualizing at least oneappendicolith: 7.7%
Increased incidence of appendicealvisualization with adequate fat
Periappendiceal stranding suggested by 1of 3 reviewers in 5% (no clinical findings ofappendicitis)
Benjaminov, etal. Radiology 2002;225:400
•Authors recommend 10.0 mm as upper limit normal
appendix if contents not visualized and no adjacent
inflammation

CT in Acute Appendicitis
Readily available, operator-independent,relatively easy to perform and interpret
Accuracy unaffected by perforation,aberrant appendiceal location, or bodyhabitus.
Sensitivities 90-100%
Specificities 91-99%

CT Technique at AEMC
1. Oral and intravenous contrast
2. Abdomen and pelvis with 5mm andthinner collimation
3. View coronal reconstructions formore rapid and confident diagnosis
•Jacobs, etal. Radiology 2001; 220:683
•Paulson, etal. Radiology 2005;235:879


CT Technique at AEMC
Rationale:
–1. thin sections improve visualizationof appendix, appendicoliths andadjacent inflammation
–2. IV contrast enhances wall ofinflamed appendix, permitting easieridentification
–3. Opacification of appendix with oralcontrast excludes appendicitis. Oralcontrast helps identify cecum andterminal ileum
Weltman, etal. Radiology 2000;216:172

Other Techniques
Focused CT of right lower quadrantafter rectal contrast
–Rao, etal. AJR 1997; 169:1275
Non-enhanced helical CT of abdomen& pelvis (better in heavier patients,optimum technique to visualizeappendicoliths)
–Lane, etal. AJR 1997; 168:405

CT Findings in Appendicitis
Inflamed appendix usually 7-15mm in diameter
Circumferential and symmetricwall thickening
Homogeneous wall enhancement
Peri-appendiceal inflammation:linear fat stranding, local fascialthickening, mesenteric haziness
Focal, cecal apical thickening
Arrowhead sign- cecal contrastfunnels to point of appendicealocclusion
Birnbaum & Wilson. Radiology 2000; 215:337



CT Criteria for Acute Appendicitis
Visualize abnormal appendix OR appendicolithwith periappendiceal inflammation
•Appearance of abnormal appendix varies withstage and severity of inflammatory process
•Most subtle findings in those scanned shortlyafter onset of symptoms- minimally distendedfluid filled structure (5-6 mm) with little or noinflammation (< 5%)
•Most have greater luminal distention and trans-mural inflammation
Birnbaum & Wilson, Radiology 2000; 215:337

Sensitivities & Specificities of CTsigns of appendicitis
Fat stranding
Appendix> 6mm
Cecal apical thickening
Adenopathy
Appendicolith
Paracolic fluid
100%, 80%
93%, 100%
69%, 100%
62%, 66%
44%, 100%
18%, 86%
(Oral and rectal contrast only)
Rao, etal. J. Comp Assit. Tomography. 1997;21:686

Appendiceal and Peri-appendicealAir at CT
Intraluminal, air bubbles
Intraluminal, A/F levels
Intraluminal, tubular
Intramural
Peri-appendiceal, air bubbles
Peri-appendiceal, A/F levels
Within appendicolith
12 30
7 2
0 25
5 0
4 0
9 0
13 0
% in Appendicitis in Normals
Rao, etal. Clinical Radiology, 1997; 52:750

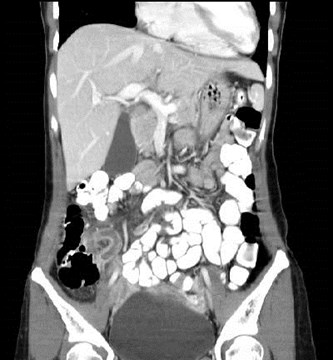
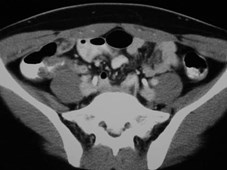
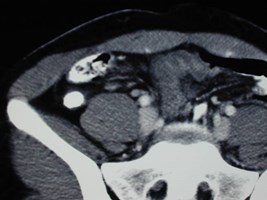
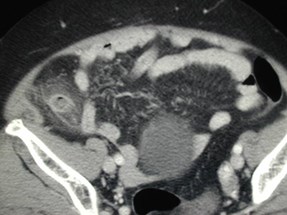
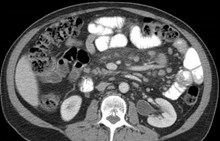
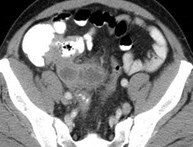
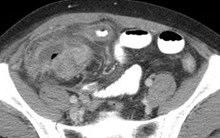
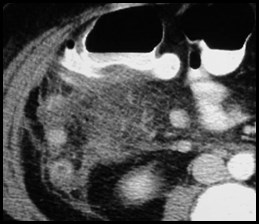
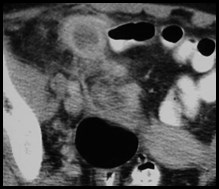
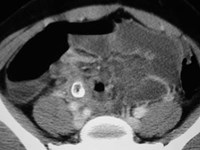
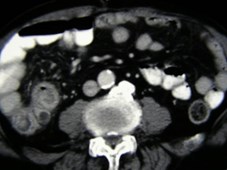
Appendicitis
Appendix posterio-lateral to cecum with enhancingwall, inflammation, and intra-luminal bubbles of gas

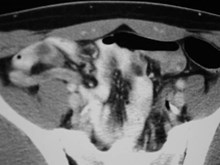
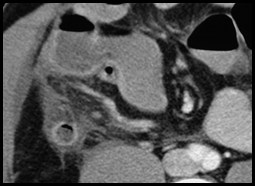
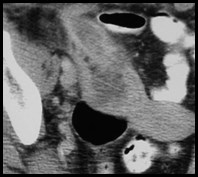
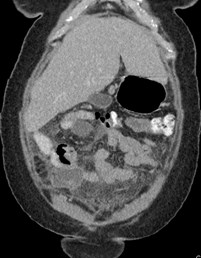
Terminal Ileum Arrowhead Sign
Periappendiceal inflammation
Enhancing, dilated appendix
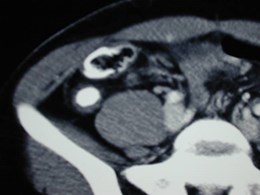
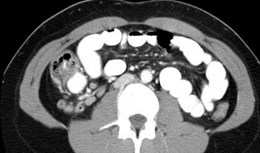
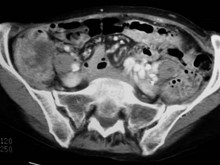
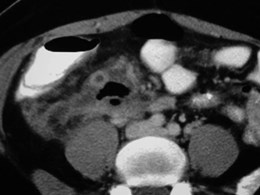
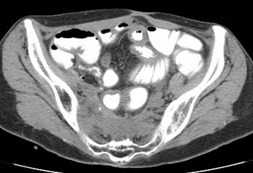
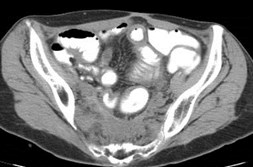
Simple Appendicitis

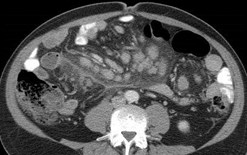
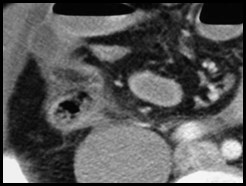
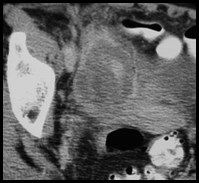
Mild Appendicitis

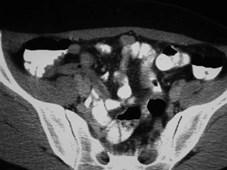
Findings: minimal
inflammation, focal cecal
thickening (cecal bar), non-filling of appendix with oralcontrast,enhancing wall,
filled with fluid, bubbles


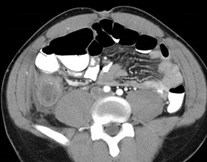
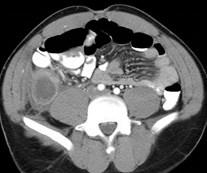
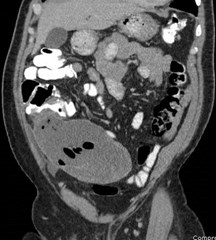
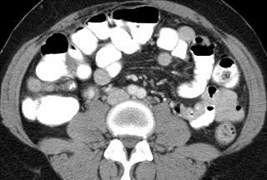
1.Thickening of terminal ileum
2.Thickening of cecum
3.Enhancing appendix with adjacentinflammation
4.Lymphadenopathy
1
2
3
4

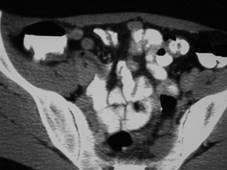
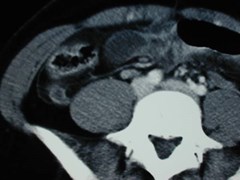
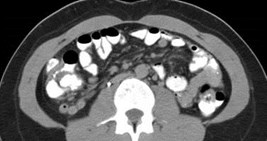
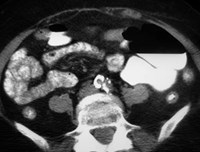
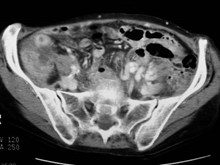
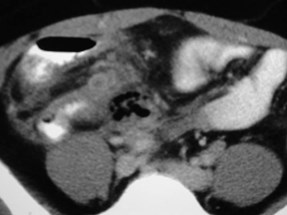
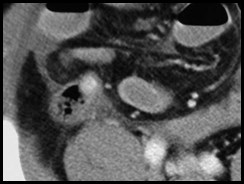
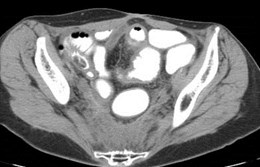
Proximal appendix normal, distal appendixobstructed and inflamed


15 year old male with RLQ pain and dysuria
Acute Appendicitis:value of contrast


What are the findings on the scout film?




Smooth, defect along medial cecum due to cecalbar and inflamed appendix

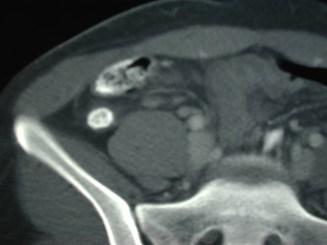
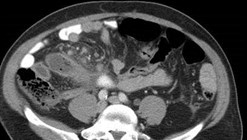
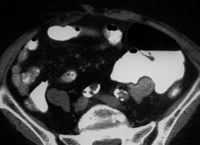
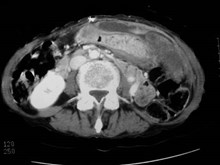
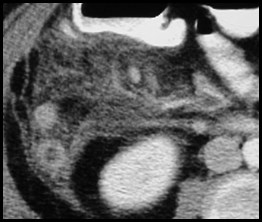
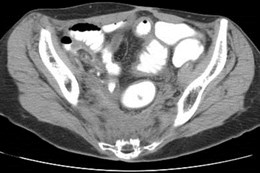
Inflamed appendix with
Simple fluid collection:
Unruptured Appendicitis

Lith at base Dilated, enhancing
of appendix distal appendix

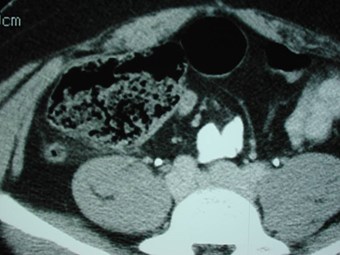
Difficult and Unusual Cases


Sagittal and coronal reformats from astone search for right sided pain



Inflamed appendix simulates small bowel loop,liths better visualized without oral contrast
N.B. Pneumatosis of appendix, extraluminal gas

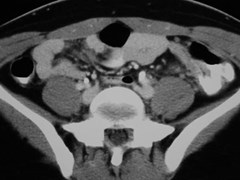
Right lower quadrant pain


Non-contrast filled inflamed appendix
Distal to large appendicolith,
initially missed



Nonspecific abdominal pain
Missed Appendicitis



One week later
Perforated appendicitis withabscess

January
August
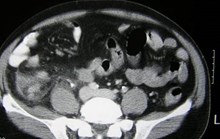
Acute Appendicitis
Normal Appendix

November
Recurrent Appendicitis

Recurrent Appendicitis
60 patients with clinical and ultrasoundpositive appendicitis were treatedconservatively, over 10 years
23/60 (38%) had recurrent appendicitis aftermedian of 14 weeks with 70% within oneyear of initial attack
The larger the appendix on the initial study,the more likely the recurrence
Cobben, Radiology 2000;215:349



Acute Appendicitis versus Mesenteric Adenitis?
One Hour Later
Acute Appendicitis with lymph nodes


Lymphoma versus Appendicitis?
Perforated Appendicitis with adenopathy




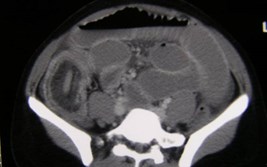
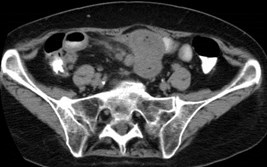
Appendicitis with Malrotation



Two other cases of malrotation: findthe appendix




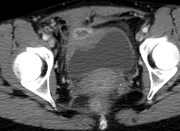
9 week pregnancy
Right lower quadrant pain
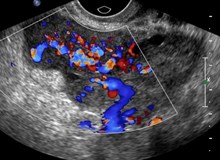
Right Ovarian VeinThrombosis



24 year old woman with right lower quadrant pain
Crohn’s Diseaseinvolving appendix




Incidental Appendicoliths

Incidental Appendicoliths
Over 4 years, retrospective review found 74patients with appendicolith who did not undergosurgery
52 (70%) had an alternate diagnosis and did notreturn
22 were discharged with possible appendicitis and5 returned with path proven acute appendicitisj
Appendicolith may be a marker for increased riskof appendicitis, but not necessarily an indicationfor prophylactic appendectomy
Emerg Radiol 2007;14:161

Chronic appendicoliths?
CT in trauma patient

Study 1 year earlier



Acute right lower quadrant pain
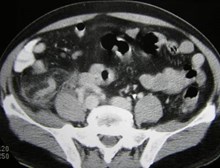
Acute Appendicitisno surgery



3 months later, recurrent pain
Simple Mucocele of the Appendix



Mucocele due to low grademucinous appendiceal tumor

Mucocele of the Appendix
Definition: A dilated appendix withabnormal accumulation ofintraluminal mucus.
–Simple mucocele due to chronicobstruction.
–Complex mucocele due to mucoidhyperplasia secondary to benign ormalignant neoplasm.
Curvilinear mural calcification isspecific for diagnosis but present in< 50%.
Intra-luminal bubbles suggest superinfection.
Appendix with mean diameter > 15-20 mm highly suggestive ofmucocele.
Bennett, etal. AJR. 2009;192:W103


Our diagnosis: Possible early appendicitis
Surgery: Lymphoma of appendix



Mucinous adenocarcinoma of the appendix


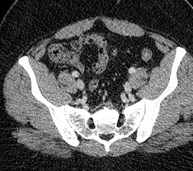
Pseudomyxoma Peritoneii secondary to mucinousadenocarcinoma of appendix

Primary Neoplasms of the Appendix
In AFIP study of 60 patients, 26 (40%)presented with acute appendicitis
Morphologic changes of neoplasm werepresent in 19/26 (86%) in additional to acuteinflammatory changes
Tumors: mucinous adenoma (29), mucinousadenocarcinoma (15) adenocarcinoma (9),carcinoid (7), lymphoma (5)
Mucoceles (generic description for cysticdilatation of appendiceal lumen from slowgrowth of tumor with obstruction) were causedby mucinous neoplasms in all but one
Pickardt. Radiology 2002;224:775





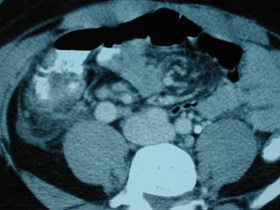
Perforated cecal carcinoma with obstructedappendix, abscess and liver metastases

CT Findings in PerforatedAppendicitis
Classic findings: abscess, extra-luminal air orextra-luminal appendicolith- 69% sensitivity ifone sign is present
Additional findings: defect in enhancingappendiceal wall, phlegmon- 94.9% sensitivityif one of 5 signs is present
Defect in enhancing wall had highestsensitivity of individual signs (64%)
Horrow, White, etal. Radiology, 2003; 227:46-51
Foley, etal. Radiology 2005;235:89-86

CT Findings in PerforatedAppendicitis
Approximately 80% demonstratedwall enhancement
Appendix only visualized in 82%perforated cases (100%- non-perforated)
All patients > 60 years withappendicitis had perforation
Horrow, White, etal. Radiology, 2003;227:46-51

Other helpful findings inperforated group
Larger appendix, though no specificcut off
Secondary findings such as cecalthickening and inflammatorystranding are worse
Strong association between degreeof periappendiceal inflammatorystranding and length of hospital stay
Foley, etal Radiology, 2005;235:89

Re-examination of findings withmulti-detector CT
Of 40 surgically proven cases of perforatedappendicitis, a defect in the enhancing wallwas found in 38 and only in 2 patients out of62 with simple appendicitis
Sensitivity 95%, specificity 96.8%, accuracy96.1%
Cine mode of transverse images most helpful
Tsuboi. Radiology 2008; 246:142

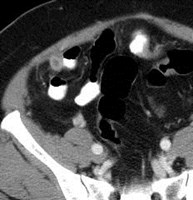
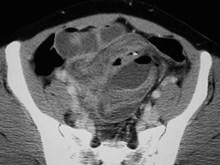
Break in enhancing appendiceal wall with adjacent
collection extra-luminal gas and inflammation
Ruptured Appendicitis

1
2
1. Intact appendix with phlegmon
2. Focal defect in enhancing wall

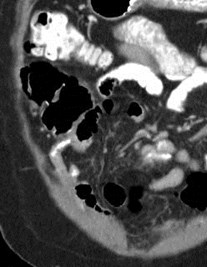
1.Focal defect in
enhancing wall
2. Larger defect
3. Extruding
appendicolith
1
2
3

1a
1b
2
1.Enhancing appendixwith defect in wall
2. Abscess


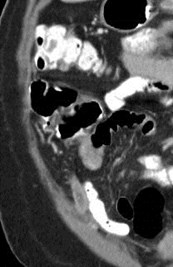
1. SBO 2. Inter-loop abscess
3. Appendicolith actualappendix not identified
Ruptured
Appendicitis



Fever and right upper quadrantpain, R/O cholecystitis
Liver Abscess



Ruptured retrocecal appendix



Liver Abscesses
Appendicitis



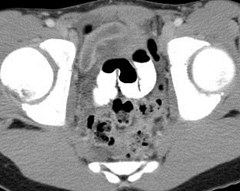
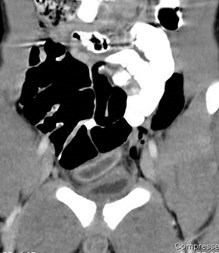
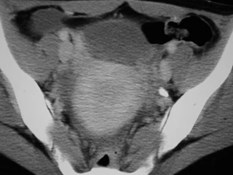
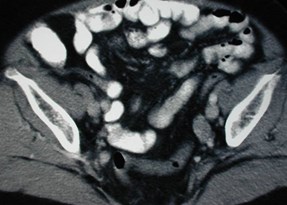
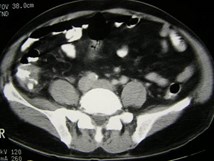
9-24 Ruptured Appendicitis


Patient returns 11/24 with pain and fever
Peritonitis with left TOA and right pyosalpinx

Conclusion
“… a dedicated search for five specific CTfindings – extraluminal air, extraluminalappendicolith, abscess, phlegmon, and a defectin the enhancing appendiceal wall – allowsexcellent sensitivity (94.9%) and specificity(94.5%) for the diagnosis of perforatedappendicitis when evaluated in a group ofpatients with known appendicitis. A defect inthe enhancing appendiceal wall had the highestsensitivity (64.3%) of any individual finding.”

Impact of CT on NegativeAppendectomy Rates
Negative appendectomy rate decreased:
22% to 4% Balthazar, eta. Am J Gastro 1998;93:768
20% to 7% Rao, etal. Ann. Surg. 1999;229:344
15.5% to 2% Applegate, etal. Radiology 2001;220:103
Before and after pre-operative CT

Non-Visualized Appendix atMultidetector CT
Of 400 consecutive patients: 80 (20%)appendicitis, 79 (19.8%) another dx, 182 (45.5%)normal appendix and no cause for pain, 59(14.8%) appendix not visualized.
50 with adequate follow-up (3 mos), 49 normal, 1with appendicitis initially scanned post partum
“Thus, in an otherwise normal MDCT scan in a patient suspected ofhaving acute appendicitis, non visualization of the appendix was negativefor appendicitis in 98%. Conversely, when the appendix was seen atMDCT and was abnormal, appendicitis was present in 95% of cases.”
Ganguli Radiology 2006;241:175
Nikolaidis, AJR 2004;183:889

Appendicitis in Pregnant Patients
Ultrasound: use high frequency transducerand graded compression
CT
MR- 51 consecutive patients, using 300 mLferumoxil and 300 mL barium sulfate toprovide negative contrast on T1 and T2,found sensitivity of 100% and specificity of93.6%
Oto, etal. Radiology 2005:234:445
Pedrosa Radiology 2006;238:891

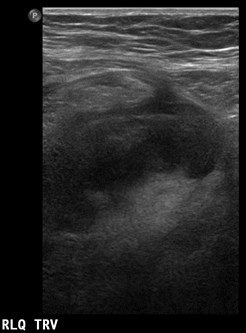
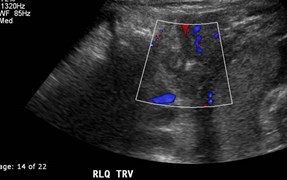
RLQ pain during first trimester ofpregnancy: normal appendix
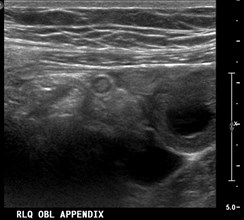
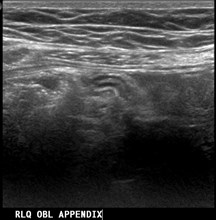
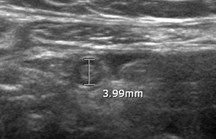

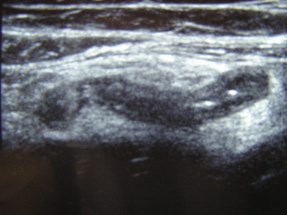

Blind ending, non-compressible tubularstructure, 7mm thickness, adjacentechogenic fat indicating inflammation
Appendicitis

Sagittal Transverse

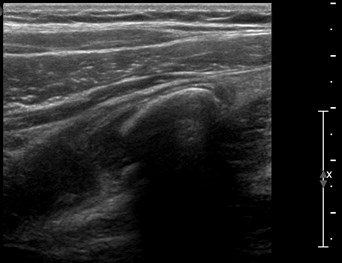
Acute appendicitis with large lith


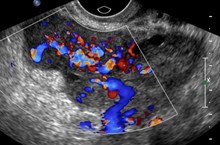
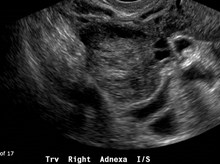
Pelvic US to rule out torsion




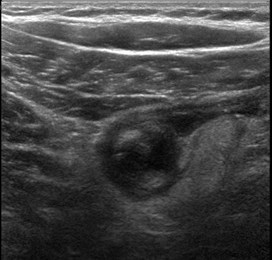
Perforated appendicitis withabscess



Acute Appendicitis inthe third trimester

Appendicitis in Pregnancy
MR should be integrated into work up of appendicitis inpregnant patients
Recent retrospective review of negative laparotomy rate(NLR) and perforation rate (PR) before and after additionof MR into diagnostic imaging of pregnant patients:
–Pre- MR, NLR = 55% with PR = 21%
–Post-MR, NLR = 29% (47% decline) with PR = 26% (statisticallyunchanged)
–Sensitivity (89%), specificity (97%) , PPV (74%) , NPV (99%)of MR imagingin diagnosis of appendicits:
Rapp etal. Radiology. 2013, published online
Doi: 10.1148/radiol. 12121027

US or CT for Diagnosis of Appendicitisin Children and Adults? A Meta-Analysis
Pooled sensitivity and specificity:
–Children: US 88/94 CT 94/95
–Adults: US 83/93 CT 94/94
“From a diagnostic performance, CT had a significantlyhigher sensitivity than did US in studies of children andadults; from the safety perspective, however, one shouldconsider the radiation associated with CT, especially inchildren”
Dona. Radiology 2006;241:83

Common Alternate Diagnoses
Crohn’s Disease-long segment TI thickening
PID- especially a right sided hydrosalpinx
Acute pyelonephritis
Urinary tract obstruction
Hemorrhagic ovarian cyst- most frequent gynecologiccondition presenting with RLQ pain
Right sided diverticulitis
Mesenteric adenitis- enlarged lymph nodes with normalappendix
Epiploic appendigitis
R colon CA with obstruction or perforation
Infectious ileocolitis: yersinia, campylobacter, salmonella
Yu, etal. AJR 2005;184:1136-1142

Uncommon Alternate Diagnoses
Mucocele: 2° post appy scarring, tumors, fecaliths
Right ovarian vein thrombosis
Ovarian dermoid: torsion, rupture, hemorrhage
Necrotic leiomyoma
Ovarian torsion
Endometriosis- involves terminal ileum, thickening,stranding
Typhlitis- length of involved cecum thicker thanappendicitis
Sigmoid colon diverticulitis
Intussusception
Yu, etal. AJR 2005;184:1143-1149

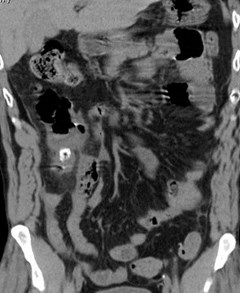
Recent review of alternative diagnosesto suspected appendicitis
Recent retrospective review of 1571 ER CT casesfor possible appendicitis
Specific diagnosis made in 55.2% of patients
–Acute appendicitis in 23.6% (371)
–Alternative diagnosis in 31.6% (496)
•204 of 496 (41.1%) with alternative diagnosis were hospitalized
•109 of 496 (22.0%) underwent surgical of image guided intervention for alternativediagoses compared to admission and procedural rates of 14.1% and 4.4% inpatients in whom a specific diagnosis was NOT made at CT.
•Alternative diagnoses: GI (46%), GYN (21.6%), GU (16.9%) andhepatopancreaticobiliary (7.7%)
Pooler, etal. Radiology 2012;265:733-742








PID with an inflamed right fallopian tube

PID versus Appendicitis?




Blind ending tubular structure: Appendicitis



Cecal Diverticulitis


Cecal Carcinoma causing obstruction of appendix

Meckel’s Diverticulum
Appendix
History of rectal carcinoma with surgery and radiation therapy

Meckel’s Diverticulum
Omphalomesenteric duct anomaly
True diverticulum with all ileal layers
Contains heterotopic tissue in 50%,especially gastric mucosa
A blind ending tubular structure arisingfrom the antimesenteric border of the distalileum
Can undergo inflammation, ulceration,perforation, hemorrhage, intussuception
Radiographics 2004;24:565


ALL, neutropenia, fever, RLQ pain
Typhlitis, resolved with medical therapy



Terminal Ileum Diverticulitis



SBO secondary to ileal-colic intussuception


Carcinoid

Ileal Carcinoid
Manifests as muralthickening,desmoplastic reactionand kinking of the bowel

Radiographics 2007;27:236

Small Bowel Carcinoid
Of all GI carcinoids, 42% occur in small intestine
Carcinoid syndrome (flushing, sweating,bronchospasm in < 10%, secondary to serotonin)
Primary tumor produces infiltrative cords whichinsinuate through muscularis propri causing a focalmass in the subserosa and mesentery. Serotonincauses desmoplastic reaction
Kinks and sharp curvatures in small bowel =“hairpin turn” secondary to infiltration and fibrosis
Transmural extension causes concentric wallthickening
Radiographics 2007;27:237


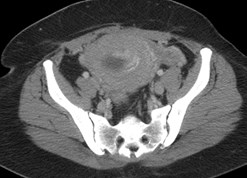
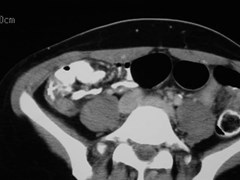
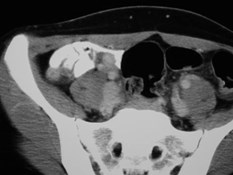
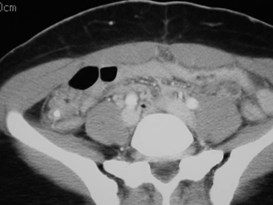
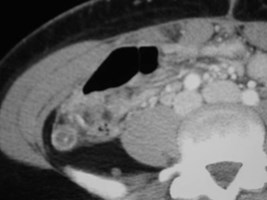
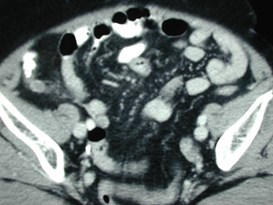
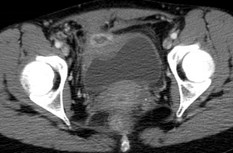
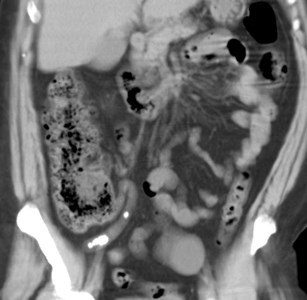
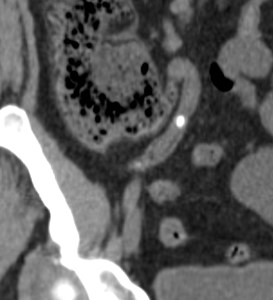
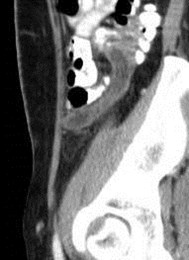
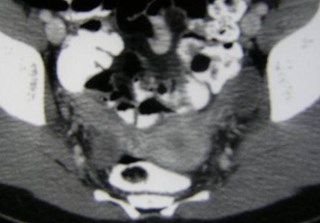
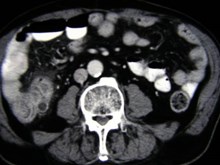
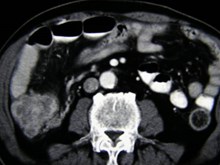
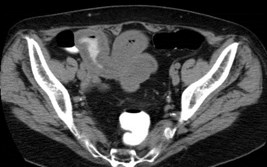
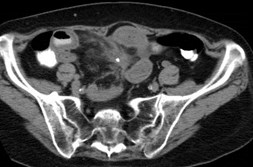
9 weeks pregnant with RLQ pain
RLQ inflammation, normal appendix


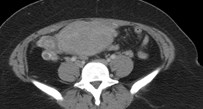
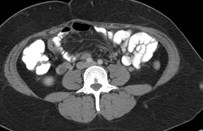
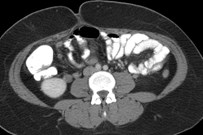
Right ovarian vein
Septic phlebitis




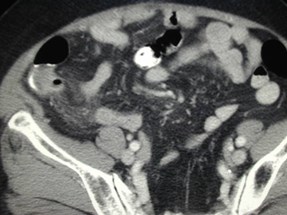
Crohn’s Disease with involvement of appendix



Kings Canyon National Park, California, August 2007
THE END